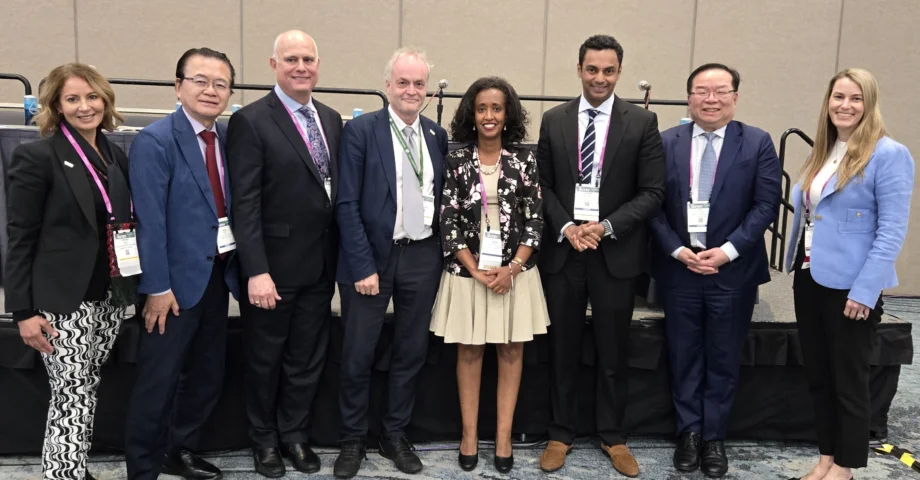
The ASGE and WEO international symposium, “Endoscopic Training : a Worldwide Perspective” took place on May 4 during DDW 2025. Five speakers from around the world shared their knowledge, experience, and perspectives, and the session was moderated by Drs. Lars Aabakken, Douglas Faigel, and Hisao Tajiri.
Training in endoscopy happens all over the world, but in a variety of formats. This may be partly due to differences in needs, but likely also for cultural and traditional reasons.
The symposium aimed to highlight some of those differences and foster a better understanding of how training can be optimized, and hopefully standardized, in a world where increasing mobility is reflected among endoscopists.
The first speaker, Prof. Catharine M. Walsh from Canada gave a presentation on endoscopy education, namely the fundamentals of skills training. She outlined best practices in teaching endoscopy skills, emphasizing structured training through a “preparation–training–wrap-up” model. Effective teaching involves setting clear learning objectives, using standardized terminology, minimizing cognitive overload, and tailoring instruction to the learner's level.
Dr. Saurabh Mukewar from India described the importance of training to spread of patient care in underserved areas. He noted that India is ready and willing to participate in this endeavor and showed examples of how Midas Hospital accepting fellows from Rwanda and preparing conditions to ensure trainees success. There are some challenges that the trainees to overcome when coming to India from Africa, including language and social customs. Future improvements will focus on the structure of the program, logistics and accommodation.
Prof. Purnima Bhat from Australia reported on the role of resources for endoscopic training in remote areas. She described that access to medical care in such areas, especially in Africa, remains a serious challenge. Current solutions include mobile services such as endoscopy buses, aircraft outreach, and local training, but these are often limited by shortages of equipment and trained personnel. Regional training must consider the long distances, limited resources, and high demand. She finally emphasized that rural healthcare – especially in Africa – must not be left behind.
Dr. Roy Soetikno from Indonesia discussed how to make the most of models and simulators in training. He explained that the ultimate goal of endoscopy education is to train learners to perform like expert endoscopists, combining technical skills with sharp observation, sound decision-making, and effective communication. Achieving this requires structured training, supported by simulators and virtual technologies; these are especially useful in the early stages when the learning curve is flat. Early involvement of junior trainees and substantial collaboration enhance the learning environment. Learning outcomes progress gradually, and education should be based on evidence, at the same time contributing scientifically to its development. He also stressed that fostering self-efficacy is essential for learners’ long-term success.
Finally, Dr. Hanna Aberra from Rwanda reported on the experience of training in Africa. She described that Rwanda faces a severe shortage of hospitals, trained doctors, and structured training programs – especially in gastroenterology and hepatology. The government of Rwanda has launched a GI Fellowship Program, which now aims to train future educators, develop subspecialists in interventional gastroenterology and hepatology, and establish a modern GI unit as well as international live training events. Future plans include expansion into radiology and colorectal surgery fellowships, positioning Rwanda as a regional training hub.
The presentations were followed by a lively question-and-answer session. Lars Aabakken summarized that all the presentations were significant because of the concrete manner in which they brought to life current situations and issues.