Colon cancer screening programs have been shown to reduce colon cancer incidence and mortality primarily through identification and removal of adenomatous lesions. While cold forceps have traditionally been used to remove polyps <5 mm and hot snare polypectomy (utilizing electrocautery) for larger polyps, interest in cold snare polypectomy is increasing. Benefits of the cold snare technique include lower potential rates of incomplete resection compared to cold forceps, and lower rates of adverse events including delayed post-polypectomy bleeding compared to thermal (hot) forceps biopsy or snare techniques.
The following represents our approach to cold snare polypectomy.
Tip #1
Once a lesion is identified, it is important to closely examine it using a combination of high-definition white light and an optical chromoendoscopy technique (such as narrow-band imaging) to identify the pit pattern, any features of deep invasion, and the extent of the lesion (Figure 1). If you are planning on proceeding with resection, place a suction trap to ensure the polyp is not lost.

Tip #2
If the borders of the lesion are not clear, consider a submucosal injection of a solution containing a dye such as methylene blue or indigo carmine to identify the borders of the lesion.
Tip #3
We generally utilize cold snare polypectomy as our primary resection modality for sessile lesions <10 mm. We consider piecemeal cold snare polypectomy after injection for sessile lesions >10 mm. For pedunculated lesions, particularly those with a large stalk, and bulky sessile lesions we generally prefer hot snare resection, to cauterize larger feeder vessels.
Tip #4
Next, identify the relationship of the lesion to the mucosa and adjacent folds. It is helpful to re-orient the lesion to the 5-o’clock position by using a combination of torque and tip deflection (5 o’clock is the position of the biopsy channel for the colonoscope so the optimal position may be different if a different endoscope is used).
Tip #5
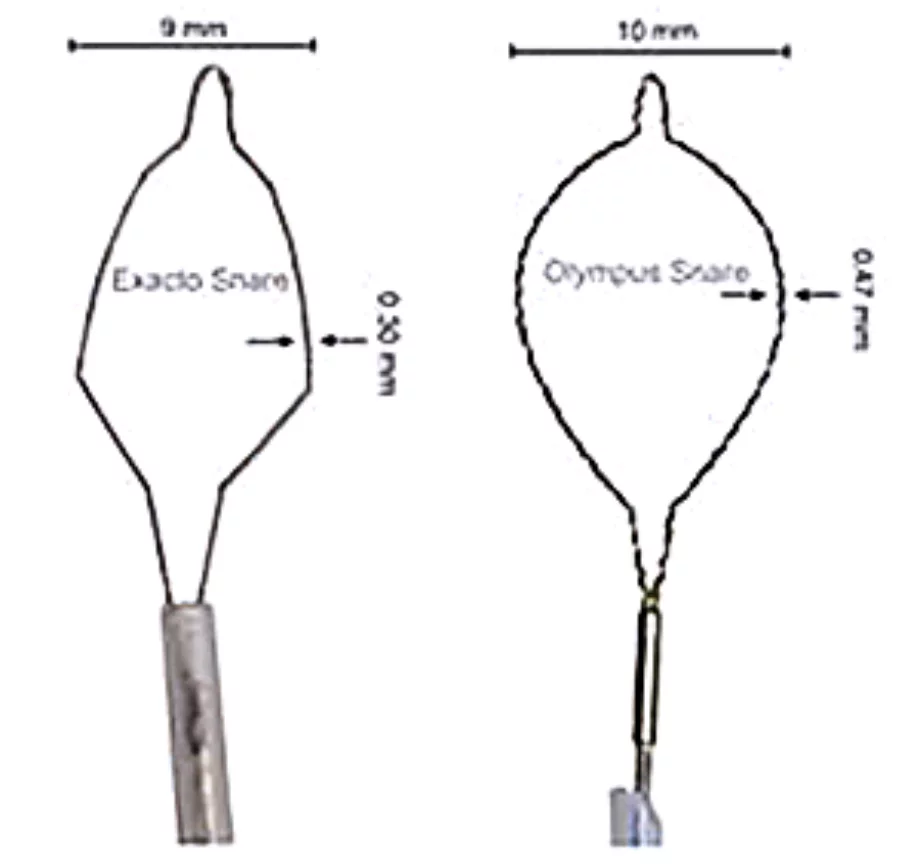
The ideal snare for cold snare polypectomy is a stiffer snare made of a thinner, braided or monofilament wire as these characteristics make it easier to flatten the mucosa and to transect the tissue, respectively. Examples of such snares include the Exacto (US Endoscopy, Mentor, Ohio, USA), Lariat and SnareMaster (Olympus America, Center Valley, Pennsylvania) (Figure 2). If you are not using a stiffer snare, it can be helpful to shape the snare by manually deforming it prior to insertion into the endoscope.
Tip #6
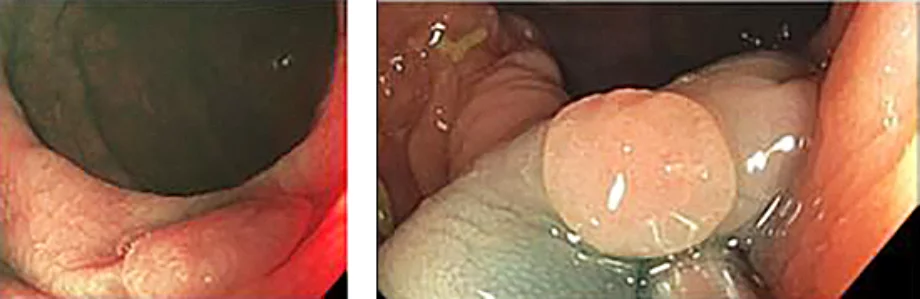
If the lesion is on the edge of a fold, consider a submucosal injection to lift the lesion and make it easier to perform cold snare polypectomy (Figure 3). Otherwise, the snare may slip over the fold (particularly if the lesion is small).
Tip #7
After the polyp is in the correct orientation, open the snare over the lesion, and use a combination of tip deflection and advancing the snare out of the channel to obtain tissue apposition, flatten the mucosa, and ensure the lesion is in the snare (Figure 4). It is helpful to have at least 1 mm of normal tissue on all sides of the lesion.

Tip #8
Once an appropriate amount of tissue is inside the snare, apply air suction and then close the snare (having the assistant close until the snare is tight around tissue) (Figure 5). If the lesion is clearly within the tissue in the snare, you can proceed with cutting through the tissue while retracting the snare into the suction channel as it facilitates retrieval.

Tip #9
If the snare is not able to close or it appears that there is too much tissue in the snare, there are several options for reducing the amount of tissue or tissue depth without losing the lesion. The easiest may be to have the assistant slightly open the snare and use a combination of moving the snare back and forth and relaxing the pressure flattening the mucosa to allow part of the tissue grasped by the snare to release. You can then re-attempt cutting through the lesion.
Tip #10
If you are still unable to cut through the lesion, consider the tug technique where the entire snare is retracted into the endoscope using the retraction to cut through the tissue. Otherwise, it may be helpful to open the snare and re-attempt or consider a submucosal injection.
Tip #11
As soon as you cut through the lesion, remove the snare and apply air suction to draw the polyp into the suction trap. If you do not have the polyp, look at the resection site as the resected tissue may have remained on it. Also, suction pools of fluid that may have accumulated adjacent to the resection site. If the specimen is still not retrieved, consider suctioning after a water flush.
Tip #12
Next, examine the polypectomy site. It can be helpful to aim the water jet at the resection site, which can expand the submucosal space and make it easier to visualize. A submucosal cord is normal (Figure 6). If there is remaining polyp tissue, it can be removed with a repeat cold snare polypectomy or cold biopsy forceps.
Tip #13
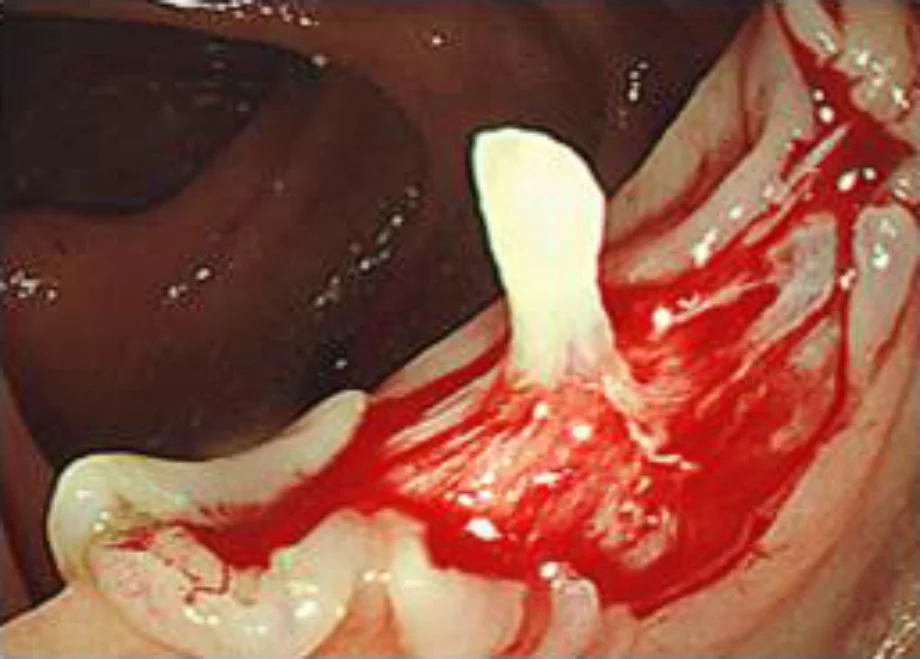
A small amount of oozing can be expected at the polypectomy site. Spontaneous cessation is observed in nearly all cases. We apply hemostatic clips if there is prolonged active bleeding from the site in a patient with known or suspected platelet dysfunction or coagulopathy (acquired or medication-related).